Parkinsons Disease

Parkinsons disease is a neurological movement disorder. Common symptoms include tremor, slowness of movement, stiff muscles, unsteady walk and balance and coordination problems. There is no cure for the disease. Most patients can maintain a good quality of life with medications. In some patients, surgery can help improve symptoms
What is Parkinsons disease?
Parkinson’s disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinson’s disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Who gets Parkinson’s disease?
About 50% more men than women get Parkinson’s disease. It is most commonly seen in persons 60 years of age and older. However, up to 10% of patients are diagnosed before age 50.
About 60,000 new cases of Parkinson’s disease are diagnosed in the United States each year.
Is Parkinson’s disease inherited?
Scientists have discovered gene mutations that are associated with Parkinson’s disease.
There is some belief that some cases of early-onset Parkinson’s disease – disease starting before age 50 – may be inherited. Scientists identified a gene mutation in people with Parkinson’s disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinson’s disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinson’s disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells’ ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinson’s disease.
Scientists think that about 10% to 15% of person’s with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
What causes Parkinsons disease?
Parkinson’s disease occurs when nerve cells (neurons) in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical (neurotransmitter) that helps the cells of the brain communicate (transmits signals, “messages,” between areas in the brain). When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brain’s commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinson’s disease.
People with Parkinson’s disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the body’s autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinson’s disease.
Scientists aren’t sure what causes the neurons that produce these neurotransmitter chemicals to die.
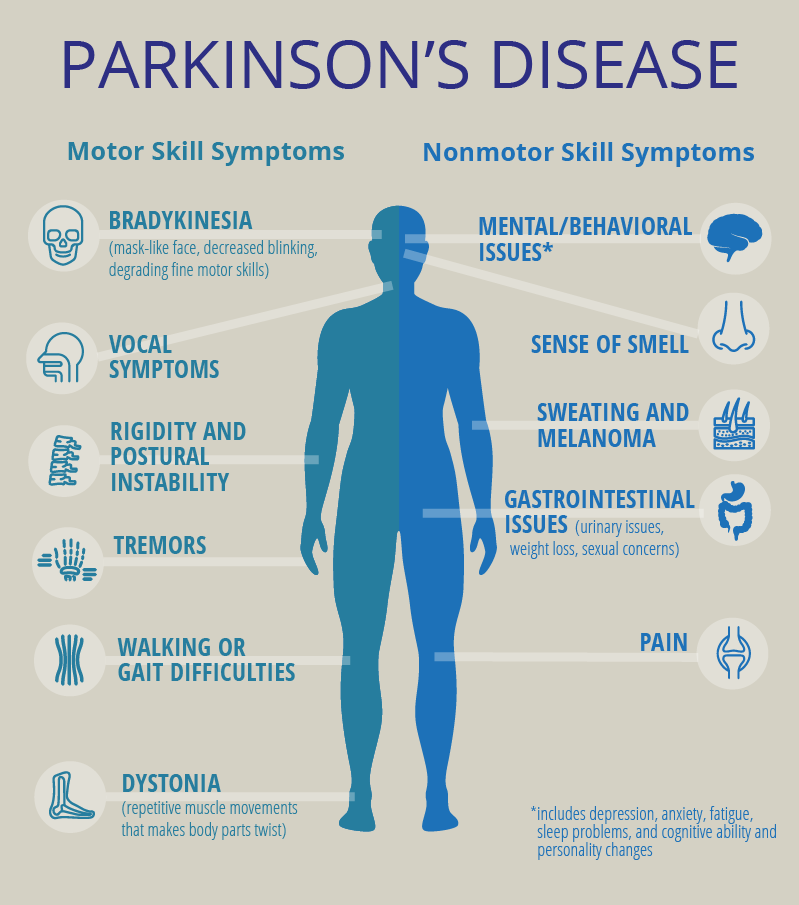
What are the symptoms of Parkinsons disease?
.
Symptoms of Parkinson’s disease and the rate of decline vary widely from person to person. The most common symptoms include:
- Tremor: Shaking begins in your hands and arms. It can also occur in your jaw or foot. In the early stages of the disease, usually only one side of your body or one limb is affected. As the disease progresses, tremor may become more wide spread. It worsens with stress. Tremor often disappears during sleep and when your arm or leg is being moved.
- Slowness of movement (bradykinesia): This is the slowing down of movement and is caused by your brain’s slowness in transmitting the necessary instructions to the appropriate parts of the body. This symptom is unpredictable and can be quickly disabling. One moment you may be moving easily, the next you may need help moving at all and finishing tasks such as getting dressed, bathing or getting out of a chair. You may even drag your feet as you walk.
- Rigid muscles/stiff limbs: Rigidity is the inability of your muscles to relax normally. This rigidity is caused by uncontrolled tensing of your muscles and results in you not being able to move about freely. You may experience aches or pains in the affected muscles and your range of motion may be limited.
- Unsteady walk and balance and coordination problems: You may develop a forward lean that makes you more likely to fall when bumped. You may take short shuffling steps, have difficulty starting to walk and difficulty stopping and not swing your arms naturally as you walk. You may feel like your feet are stuck to the floor when trying to take a step.
- Muscle twisting, spasms or cramps (dystonia). You may experience a painful cramp in your foot or curled and clenched toes. Dystonia can occur in other body parts.
- Stooped posture. You have a “hunched over” posture.
Other symptoms include:
- Decreased facial expressions: You may not smile or blink as often as the disease worsens; your face lacks expression.
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged (monotone).
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Chewing and swallowing problems, drooling.
- Urinary problems.
- Mental “thinking” difficulties/memory problems.
- Hallucinations/delusions.
- Constipation.
- Skin problems, such as dandruff.
- Loss of smell.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest (apathy), fatigue, change in weight, vision changes.
- Low blood pressure.
What are the different stages of Parkinsons disease?
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement (no arm swing when walking) slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Symptoms start getting worse. Tremor, muscle stiffness and movement problems may now affect both sides of the body. Balance problems and falls are becoming more common. You may still be fully independent but daily tasks of everyday living, such as bathing and dressing, are becoming more difficult to do and take longer to complete.
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
You now require a wheelchair to get around or are bedridden. You may experience hallucinations or delusions. You now require full-time nursing care.
How is Parkinsons disease diagnosed?
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT (computed tomography) or MRI (magnetic resonance imaging) scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
How is Parkinsons disease treated?
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
What medications are used to treat Parkinsons disease?
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.